Case studies
When Dr.Deepak Shinde was walking on the platform early in morning.He saw a girl lying on the platform and her friend sprinkling water on her face thinking she was fainted.Out of curiosity he checked her.She had no pulse,her breathing had stopped and she was not responding.Concluding she had cardiac arrest he started doing cardiac massage.With the help of coolie she was lifted to police van which could take them to nearby hospital.While being in the ambulance he continued to do give cardiac massage.After reaching the hospital in span of five minutes she was immediately given DC shock and gave her intavenous adrenaline and put the patient on ventilator.Over next one week patient was hemodynamically stabel and re-attained her conciousness fully.She was found to have hypertrophic cardiomyopathy as a cause of cardiac arrest and was later underwent AICD (automatic device which can give direct shock and prevent cardiac arrest)
Past medical history (PMH)
Hypertension, atrial fibrillation, coronary artery disease, stroke, congestive heart failure.
Medications
Metoprolol, digoxin, ASA (aspirin), lisinopril, furosemide (Lasix), Coumadin (warfarin), esomeprazole (Nexium).
Physical examination
In pain, combative and confused.
VSS.
Chest: Occasional bibasilar crackles.
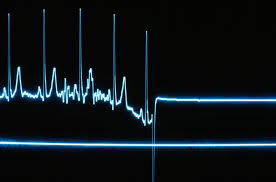
Cardiovascular System: Clear S1 and S2, irregularly irregular rhythm, HR 101 bpm.
Abdomen: Soft, epigastric tenderness, no rebound, + BS.
Extremities: No edema.
What is the most likely diagnosis?
Digoxin toxicity.
What would you do?
Stop digoxin.
Monitor digoxin levels.
Control symptoms.
Sitter in the room.
What happened?
The initial digoxin level was elevated at nearly twice the upper therapeutic level. All symptoms resolved as digoxin level decreased to therapeutic range. Heart rate was controlled by increasing metoprolol dose. She was discharged back to the nursing home in good condition.
Final diagnosis
Digoxin toxicity.
Summary
Digoxin toxicity was first described in 1785.
Approximately 0.4% of all hospital admissions, 1.1% of outpatients on digoxin, and 10-18% of nursing home patients develop toxicity. Advanced age ( older than 80 years) is an independent risk factor associated with increased morbidity and mortality.
Serum concentrations associated with toxicity overlap between therapeutic and toxic ranges because of the many factors which can potentiate digoxin toxicity.